
Today's podcast features Dr. Justin Marchegiani and Evan Brand breaking down the 5 causes of leaky gut and how to fix it. Listen to this discussion if you want to get a full understanding of what a leaky gut is. Dr. Justin explains all about digestion thoroughly in this interview. They also talk about the importance of chewing your food when you eat for the digestive process.
 Learn about the connection of leaky gut to stress and cortisol. Discover an effective way to deal with leaky gut with the Dr. Justin's 5R Approach — a combination of removing bad foods, adding in digestive support, adding in healing nutrients and adrenal support, removing any infections, and bringing back and trying to repopulate with a lot of good bacteria.
Learn about the connection of leaky gut to stress and cortisol. Discover an effective way to deal with leaky gut with the Dr. Justin's 5R Approach — a combination of removing bad foods, adding in digestive support, adding in healing nutrients and adrenal support, removing any infections, and bringing back and trying to repopulate with a lot of good bacteria.
In this episode, topics include:
2:44 Digestion 101
7:45 Causes and culprits of leaky gut
11:43 Stress and cortisol
14:45 5R Approach
26:51 On testing for leaky gut
![]()
Podcast: Play in New Window|Download
Dr. Justin Marchegiani: Evan, Dr. J here. What’s cooking, man? It’s Friday.
Evan Brand: Hey, it is Friday. I didn’t cook anything for breakfast today. I just did a couple of slices of some organic simmer sauce chicken that I found that is really delicious and then I had my all-time favorite Love Crunch organic nut bar. It’s got some organic cashews, a little bit of dark chocolate, some hemp seeds, a little bit of pink salt I believe or sea salt in there, so I’m feeling macro-nutrient balanced to start my podcast here with you.
Dr. Justin Marchegiani: That’s great. I’m actually doing a little bit of intermittent fasting this morning, just did actually a little bit of Bulletproof coffee here and I’ll probably have some collagen here in a few hours, but doing a little IF this morning and I’m feeling pretty good. I’m not seeing patients ‘til this afternoon so I’m–I’m rocking it.
Evan Brand: That sounds good.
Dr. Justin Marchegiani: Very good. Well, anything else on your radar screen?
Evan Brand: Well, I’m definitely–off-topic–but I’m definitely interested in cars now. You know, I’ve been spending time off air talking about cars this morning so that’s always fun.
Dr. Justin Marchegiani: Always fun stuff, like it. Well, today we talked about digging in to leaky gut. We’ve done some videos on digestion and infections and hydrochloric acid which all play a role into leaky gut, but I think we need to do a really, you know, a good job just kinda tying everything together to really what is a leaky gut.
Evan Brand: Sure, that sounds good. For me, you know, everybody pretty comes in the door and they diagnose themselves with leaky gut. It’s like, “I have leaky gut and that’s why I’m coming to get help.” And a lot of people do have it, but I guess I wouldn’t always jump to conclusions about that, so maybe should we break down kind of like the gut a little bit? I mean, you want some level of permeability, like you have a certain level of intestinal permeability, but it’s when you’re exposed to gluten and these other things that you’re gonna increase that permeability and now toxins that should not be able to get through and infections and stuff that shouldn’t be able to get through this lining, now they can and they break through the tight junction and then now you have whether it’s an autoimmune disease or you have other physical symptoms that hurt you and then you’re troubled and then now you have to try to work on sealing that back up.
Dr. Justin Marchegiani: Yeah, absolutely. So our gut–inside of our intestinal tract is actually considered outside of our body, just kind of a weird thing to wrap your head around, so when you’re eating something, it’s technically considered outside of your body in the intestinal tract and basically we have to bring it in via the tight junctions and that gastrointestinal kind of barrier system. So we take food in, it goes into our stomach. Just kind of Digestion 101 here. We take foods into our stomach and the first level of digestion actually happens with the teeth, right? We’re breaking things down. We’re chewing–the technical term is mastication–medicine loves making big words that make no sense, so we’re masticating our food, we’re breaking it down. That starts the digestive juices being secreted. It enters our stomach and it’s starting to get churned up and the hydrochloric acid comes out which has almost like a sterilization effect with the food but also activates a lot of our proteolytic enzymes in our stomach, one known as pepsin which helps start breaking down protein. And then all that food gets mixed up into this kind of soupy mixture called chyme. And that chyme is the–should have a nice low pH and that low pH and that chyme is actually going to be released from our stomach into the small intestine and once it’s released, our pancreas spits out a whole bunch of bicarbonate to kind of bring the pH back up so we don’t have an ulcer in our small intestine, but that nice low pH initially triggers our pancreas to make a whole bunch of enzymes like trypsin and chymotrypsin and lipase, these are fat enzymes and protein enzymes that will help break down protein and fat, and it will also trigger out gallbladder to contract and spit out a whole bunch of bile salts which will start helping to emulsify fat. So the first domino is good healthy mastication in the–in the mouth by chewing that increases surface area. The stomach does its job with the–the nice pH and having a sterilization effect and also activating proteolytic enzymes, small intestines now triggered where bicar–bicarbonate comes out and then also enzymes from the pancreas and bile salts from the gallbladder. So that’s kind of where we’re at. Any questions there, Evan?
Evan Brand: No, that’s good. I mean, a lot of people, they don’t actually chew their food that well and then they wash it down with a soda or other type of drink. They’ll just put a bite in their mouth and then they’re just chugging something down and goes to the gut and you’re creating a lot more stress for the stomach. It’s gotta work harder than it should have to, so that kinda wears you out, too.
Dr. Justin Marchegiani: Yeah, I remember back in the day, this was like maybe 10 years ago when I was a personal trainer, and I was thinking that, you know, eating the conventional way was healthy and I was sitting there and I’m eating a Subway sandwich thinking that this is such a great thing, right? Because, you know, Jared from Subway lost all this weight. I’m gonna do the same thing. So I’m eating that sandwich and the roommate–my roommate next to me went and said, “You just chewed that thing 7 times before you swallowed it.” And I was like, “Whoa!” And it kinda hit me, like the first part of digestion with that stomach–with your, you know, getting the food in your stomach, chewing is so important. I think that’s a really important thing, you know, a good rule of thumb is you chew your food for every tooth that you have. So on average that should be like 32 chews or 33 chews, if I remember my dental anatomy correctly, probably 32 because it’s even. Again, if you’re unhealthy and you have no teeth, that doesn’t give you the excuse to just swallow your food whole but I think you get the idea. Chewing is super important for the digestive process.
Evan Brand: Yeah, definitely.
Dr. Justin Marchegiani: So we chew our food up, right? We get the protein digestion in the stomach. We get the fat and protein in the small intestine via the pancreas and the gallbladder. Now that food has to get broken down, ideally even more into its individual constituents, meaning protein is like the pearl necklace. Each individual pearl is like the amino acids, right? So we wanna take that pearl necklace, we wanna break it open so all those individual pearls are–are laid out so our body can then absorb the amino acids and protein digestion is very energy intensive, so if people are under a lot of stress, it can take energy-digesting proteins. So sometimes if we are in a catabolic state, our body is breaking down a lot of tissue and we’re already having digestive problems, getting free form amino acids in your digestive system that are already broken down can take a lot of stress off the gut because it can just absorb those individual pearls because they’re already broken off the necklace if you will.
Evan Brand: Yeah, so do you do capsules or do you do liquids when you are gonna do some amino acids? What do you like?
Dr. Justin Marchegiani: Typically, a combo of the two. Typically, a really good high quality protein powder in the morning, like a pea or a beef protein powder. People who are less sensitive, maybe a grass-fed whey, and then individual amino acids that are free form, because even pea and whey and beef they aren’t free form. There’s still a little bit of digestion that’s involved but, you know, not even close to the same as food.
Evan Brand: Yeah.
Dr. Justin Marchegiani: But when we have people that are showing either low amino acids on their blood work or on their organic acid test, we’ll give them additional capsule versions of free form aminos, so they bought–so they can absorb a lot of those things to help make their neurotransmitters and their–their lean tissue as well.
Evan Brand: Yeah, so unless you have a different direction to go with this thing, we should probably talk about some of the causes and culprits of leaky gut. So for me, huge–a lot of people that I talk with, who are doing CrossFit and other intense exercise and they’re depending on Advil and ibuprofen and Tylenol, and all of these other NSAIDs that are just not good for the gut lining at all, and I find that a lot of these people, once they start using these products for their pain to cope with their exercise routine, now they’re joints are hurting worse than ever before.
Dr. Justin Marchegiani: Yeah, it’s like, “Huh.”
Evan Brand: And then we start to make the connection with, “Man, that gut is getting destroyed and now other things are getting through that barrier that should not be.
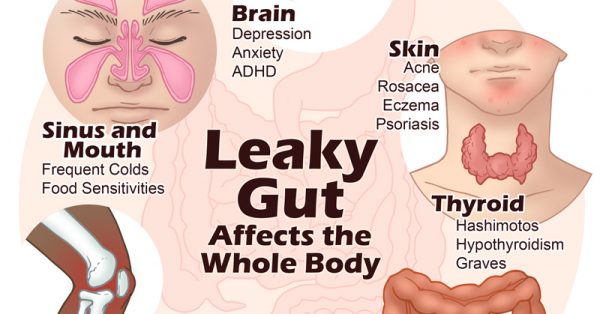
Dr. Justin Marchegiani: Uh-hmm. Exactly. So medication is definitely gonna be a stressor because it can wear down that gut lining for sure, and again, I was really stressing the digestive component because if we’re not digesting our foods down fully, what starts to happen is these proteins that are incompletely digested, they start getting into the bloodstream not in their free form, not in their essentially fatty acid form but, you know, impartially broken down or partially broken down or partially emulsified, or partially digested, right? And that’s a problem because then the immune system can freak out. It starts to say, “What’s this here? This shouldn’t be here. What’s going on?” And those surface proteins on some of those foods can resemble other body tissue. So if you look at like a–a surface protein amino acid sequence of gluten, it may resemble things like the myelin tissue that coats the nerves or it may resemble the thyroid tissue or it may resemble joint tissue. Or if you’re looking at dairy, it may resemble tissue on the pancreas for type 1 diabetics. So the foods being incompletely digested is a big component. So everyone kinda, while they’re sitting here, just put your hands together like you’re saying a prayer, right? But then you’re looking inward on the inside of your hands, so you can see the fingers interlace and you can see really tight, but you can see a nice little seam there. That’s kinda like you’re gut lining and where those fingers interlay, that’s called our tight junctions. That’s like the epithelial tissue in our gut lining and if we just pull our tissue or pull our hands apart just enough to create a little bit of daylight, that starts to hap–that’s what’s happening when we start to have a leaky gut, and again the leaky gut could be one, from eating bad foods, right? Eating foods like gluten or dairy, like dairy maybe being higher casein dairy like cheese or–or milk, or could be eating things that–higher sugar foods. They could be from infections like fungal overgrowth or parasites, or it could even be people that are sensitive like phenols and salicylates or mycotoxins that are in the food. It could even be from lack of nutrients like zinc. It could also be from you not chewing your food well or you eating while you’re having a whole bunch of stress so you’re not digesting food, so you’re not having enough enzymes or hydrochloric acid. So there’s a whole bunch of things, right? Medications you also mentioned. So all of these things. If you’re having your hands tied together, it’s like pulling them apart just a little bit and it’s allowing those undigested, unbroken down foods in those pearl necklaces that should be broken down to go into the bloodstream and then our immune system is looking for the APB, right? All posted bulletin, right? We got a–a person driving a black Lexus, it’s stolen, but then hey, the guy maybe driving the black BMW gets pulled over instead, right? It’s that case of mistaken identity and other tissues get caught up in the collateral damage and that’s what happens with leaky gut and other parts of the body. It’s that these parts of the immune system are revved up because the amino acids on these foods look similar to other tissues.
Evan Brand: That’s mind-blowing, isn’t it?
Dr. Justin Marchegiani: It is, isn’t it? I’m gonna take a breath right now and let you break some stuff down.
Evan Brand: Yeah, for sure. Well, I wanted to talk about cortisol a little bit, too, because stress is a huge part that can contribute to leaky gut and, you know, if you go back far enough in a–in a client’s history and you find that they did start doing like a CrossFit exercise or they had a significant job change or they went through a divorce or something like that, some type of huge stressor whether it’s emotional, chemical, physical, they seem to derail themselves.
Dr. Justin Marchegiani: Yes. Uh-hmm.
Evan Brand: So now, there’s that–the link between the cortisol and the leaky gut. So if you have all these other things that you’re putting in your mouth and alcohol is another big one, too. You’re putting all these things in your–your mouth that are causing you issues and you have all the stress on top of it is really when the Jenga game starts too fall. You pulled out one too many pieces of the puzzle and now the whole thing has collapsed and then you have more issues, so stress for me was a huge part of my recovery process after the diet picture was–was dialed in.
Dr. Justin Marchegiani: Yeah, and we have this kinda like this nice little balance with cortisol. It’s kinda like the Goldilocks effect, not too hot, not too cold, not too high, not too low. Cortisol goes too high, we actually burn through a lot of our gut lining. That’s stress, right? You’re under a lot of stress. That increases cortisol. You’re burning down that gut lining. You’re IgA, that’s the mucosal membrane barrier that lines the gut starts to weaken. The mucus layer on the intestinal tract or on the stomach starts to think out and then you don’t have the protection from the stomach acid and you need–too much acid will–will break down that gut lining so then when foods come in, it’s like–boom–now they can easily pass through or there could be impaired digestion. But if our cortisol’s too low, we actually need some level of cortisol to build up our gut lining, to create out gut lining and we need some level of cortisol to deal with inflammation. So little fires will maybe be ignited in our gut and if we can’t put those fires out with the cortisol, that’s gonna be a problem. And then also we need cortisol to build up that gut lining, too.
Evan Brand: So let’s go a little deeper with that and try to apply this to the stuff that we see all the time. Most people we see are low in cortisol because they’ve gone through so much stress that now they’re more like a stage 2, stage 3 adrenal fatigue. So what you’re saying here is you go high cortisol at first, so you’re stage 1. You’re burning the candle at both ends.
Dr. Justin Marchegiani: Yes.
Evan Brand: So you’re destroying the gut, right? So then they wear out the adrenals and the pancreas and the liver, all the–the whole system here and now they’re low cortisol. So now you’re saying once you hit that point, you don’t even have enough stress hormone to build these processes back up which is why you have to get the adrenals going. You have to get the digestive system going. You have to get the detox going. You’re saying, because if you don’t have enough fuel, because your stress bucket’s empty, you can’t even build this gut healing process back up anyway. Am I–am I–
Dr. Justin Marchegiani: Correct.
Evan Brand: Saying that right?
Dr. Justin Marchegiani: Correct. So once you get into this place where the gut’s starting to become leaky. You really have to then follow a 5R approach, which we’ll talk about in a bit to get the gut healed again. And that’s a combination of removing bad foods, adding in digestive support, adding in healing nutrients and adrenal support, removing any infections, and then also bringing back and trying to repopulate with a lot of good bacteria.
Evan Brand: Uh-hmm. It’s funny, I always hear, like you’ll–you’ll–sometimes the functional medicine thing, you’ll hear 4Rs and then you hear 5Rs, and then sometimes you hear 6Rs, it’s like how many are there?
Dr. Justin Marchegiani: I know right? I made up my own and the reason why I did it is because I found a lot of the order was messed up, meaning a lot of people will say remove, but they’ll say remove the foods and they’ll put the infections in the same place, and the problem with that is people–or I should say–functional medicine practitioners and doctors really screw this up because they take a sick patient who can’t regulate inflammation, they can’t digest foods, they’re already inflamed, and they go after a massive infection. There’s a whole bunch of die-off or Herxheimer’s reaction, which is the body becoming overwhelmed of the dead debris, having to process the dead debris from the in–of the–the infection killing program. It has to push it out to the limb for the detox or the kidneys or–and then the immune system has to deal with all of the–the biotoxins of the infection and the person has a healing crisis. They just feel like crap and then they fall out of the program and then there’s a patient that thinks functional medicine isn’t gonna be able to help them.
Evan Brand: Yeah.
Dr. Justin Marchegiani: So my goal is the removal of the infection is one of the last things that we do because we have to get the person digesting. We have to cut the crappy foods out. We gotta start shifting their body into an anti-inflammatory state. I gotta give their body the extra nutrients. We also have to work on giving the extra repairing nutrients so I focus at least one to two months on that before we knock out the infection, that’s why there–we have remove twice. It’s removing the beginning with the foods and then remove at the end in the fourth R with the infection and then also my third R where we do repair. Repair typically with most doctors is just healing nutrients and those healing nutrients are like the aloe, the deglycerides, licorice, the L-glutamine, a lot of these healing mucilaginous and nutritive-based amino acids, that’s the repair part. But with me, I also add in the adrenals because cortisol’s important for gut-healing and like you said Evan, most of our patients are stage 3, their cortisol’s beneath that 23 nanomils per liter on the cortisol rhythm test for their cortisol sum for the day, so they don’t have enough cortisol to even deal with the inflammation in their gut. So with us, it’s really the 5Rs and it’s–it’s that way because of thousands of patients that I’ve treated and I found this is the magic sequence that tends to work the best in most people.
Evan Brand: Well, it makes so much more sense. I mean, how could you come in with this big sledgehammer and this gut-killing protocol? I just had–actually had a–a call the other day with a girl where she’s got Hashimoto’s which is so common and she started working with another lady on top of me because she’s local, so she’s able to go see her in person.
Dr. Justin Marchegiani: Too many cooks in the kitchen.
Evan Brand: That’s what’s happening, man. So here I am trying to work on the adrenals with this lady and next thing I know, she says, “Hey, Evan. I’m taking like 10 or 15 new supplements,” and she’s on this huge gut-killing protocol now because this other lady–
Dr. Justin Marchegiani: Oh, man!
Evan Brand: Is doing it the–I almost call that like the standard functional medicine way so now, you know, she doesn’t know who to go to for all these new symptoms that are coming up because she’s taking all of these gut-killing stuff. I mean, the oregano oil, the GIX micro whatever, I mean, she’s–she’s going deep in the rabbit hole and my explanation, I try to keep it as simple as possible, as like, “How are you gonna put the windows in your house if you don’t even have the walls up yet?”
Dr. Justin Marchegiani: Oh, my gosh! You know, I totally hear you and this is the biggest mistake most functional medicine doctors and practitioners make. So anyone that’s looking for a functional medicine doctor, make sure you interview them regarding this process, because I think if they don’t have this down, then there’s probably another–you know, other pieces to the puzzle that are probably missing.
Evan Brand: Well, what–what’s happening now is that she is getting stagnant, so I mean we–we looked at the adrenal picture again and we went over some of the symptoms just on a questionnaire and it’s like, “Okay, we’re clearly reducing some of these adrenal things,” where she’s not waking up in the middle of the night anymore and things like that, but now all of a sudden with this Herx’s reaction, now the joints hurt. Now she feels like she has the flu all the time and it’s significantly reducing her confidence to continue on because she’s this early in the game with this lady and now all of a sudden everything’s getting worse, so–
Dr. Justin Marchegiani: Right.
Evan Brand: I guess, my point is here that I mean, I’m just seconding what you’re saying, it’s gotta be done in something a little bit more common sense than just coming in and killing everything just because you’ve identified something. I mean, yeah, we definitely wanna identify and that’s what we do, is identify what’s going on but we’re not gonna come in and chase after that stuff if you’re not ready for it.
Dr. Justin Marchegiani: Exactly. Exactly. So looking at the 5Rs that I’ve–you know, applied in my clinic and practice, there are a couple of exceptions. I’m gonna walk you through the exceptions. So the number one, the first exception is while we’re doing the killing, some people may need some detox or binder support. So we may add in some extra clean, you know, soluble fibers to help with binding that can have apple, pectin, or celery root or carrot root and try to do a lot of plant-based fibers that are soluble and try to avoid a lot of that–the grain-based non-soluble fibers just because of gut irritation. So that’s one extra piece to the puzzle. The next piece to the puzzle is some people do better with some probiotics during the whole program and we have a couple of different strains that we use in the office that are very helpful but we talk about the reinoculation kind of being that fifth R, that fifth phase, and that’s important and most of people will be able to do it that way, no problem. Some may need a little bit of probiotic during the program because it will help some of their gut inflammation, right? There’s been studies showing that probiotics taking can actually decrease cortisol levels in the gut and if under a lot more stress, that may be beneficial. It can also help with digestion. It can also help easing stomach inflammation and irritation, and if you’re–maybe have constipation or diarrhea, it could make a–a benefit, have a beneficial effect on some of those gut symptoms that may already be present. So depending on where that person is at, we may add some probiotics, some specific-strains whether it’s a soil-based or some specific others that we use like in the bacillus family that really help modulate any of the gut symptoms that may be present.
Evan Brand: That’s beautiful. I love how that works. I mean, it’s almost like an adaptogen, probiotics in a way. It’s like if you’re–if you’re having diarrhea, it can help balance that out. If you’re having constipation, it can help get things moving. I love the–the effect. I’m gonna put probiotics in the adaptogen category now.
Dr. Justin Marchegiani: I know right? So looking back here with the leaky gut, right? We pull apart our hands or our fingers and where they’re interlaced there, that’s where the leaky gut starts. That’s the tight junctions. Now what facilitates that is a protein called zonulin. So everything we’re doing is trying to reduce stimulation or production of zonulin because zonulin’s kind of that–the energy that pulls that gut junction apart. So gluten is the–one of the biggest stimulators of zonulin. Also endotoxin which is a toxin secreted by bacteria. The outer layer of the bacteria that has these little kind of like fla–flagella-like projections if you will–I’m making these little hand motion on the Skype, too bad everyone can’t see me on that–but these little flagella-like projections that sit off of it and now those are actually LPS, and if you google LPS, it’s another word for endotoxin. And you break endo–endo means internal, right? Toxin is toxin, right? So medicine again using big confusing words, so it’s an internal toxin produced by the bacteria that has–has to go and get filtered up by the liver, so it’s toxic. So that can actually create an increased zonulin proteins. Also things in the food, casein could be a stimulator, phenols and salicylates which is what’s kinda taken out of the GAPS diet or the SCD diet. So those can be a big thing as well and then mycotoxin and mold and even dysbiotic bacteria where your gut bacteria is really out of–out of whack and even SIBO or small intestinal bacterial overgrowth, which is another form of dysbiosis specifically in the small intestine.
Evan Brand: So you got me thinking here–
Dr. Justin Marchegiani: Go ahead. Yeah.
Evan Brand: Let me–let me interrupt you here, so, you know, talking about this endotoxin here and you’re talking about the liver’s job to get that stuff out. Let’s say someone had been taking a lot of pharmaceuticals or they have had a bad skincare regimen, where they’re getting a lot of chemicals and their diet there, maybe they are eating chemicals and other fungicides and pesticides from non-organic produce, things like that, and they’re increasing that liver burden, that could technically make the leaky gut problem worse because now you’re not able to get rid of that endotoxin as well because the liver’s focused on these other chemicals. Is that accurate?
Dr. Justin Marchegiani: Exactly.
Evan Brand: That’s scary.
Dr. Justin Marchegiani: Exactly. Uh-hmm.
Evan Brand: I mean, that’s why the foundations of this removing as many chemicals from your life is gonna be important for people listening.
Dr. Justin Marchegiani: Yeah, any stressor is–that you add to your intestinal tract is gonna be an issue because everything that goes into your gut has to go to the hepatic portal vein which then goes to the liver, and then goes filtered out and then goes systemically. So the more stress in your gut, it eventually goes to the liver as well. So the cleaner–the cleaner food that you put in your intestinal tract, the less hard–I should say–the more, I should say, what’s the better word here? The liver is not as stressed as much during the filtration process.
Evan Brand: Yeah, right. Just taking the load off.
Dr. Justin Marchegiani: Just taking the load off, that’s it and that’s important because our liver really has to work hard with all the toxins in our day and age. And I heard this at a conference recently–I’ll put it out there–I’m not sure how accurate it is but from what I understood is a healthy liver functions at 99.9%, you know, upwards of 99 in change. I heard a cirrhotic liver, a liver that’s not functioning well, it’s really only a 10% difference in its function. It’s functioning basically at 90%. And I could be wrong on that, I heard it the doctor–the doctor lectured on that topic but from what I understand, it’s only a 10% difference in filtration that makes the difference of a diseased liver and a healthy liver.
Evan Brand: Geez. So if you’re 1 or 2% off, holy crap.
Dr. Justin Marchegiani: I know, that could be a pretty big deal and that could create a lot of symptoms, too.
Evan Brand: Yeah, so it means–something that’s kinda like the overwhelming idea of this whole thing is that it’s not one thing, you know, everybody’s always looking for that one thing that’s gone wrong that’s caused their health issues, it’s not one thing. It’s a combination of things. Like I told you, I had a cankersore that popped up in my mouth, you’re like, “Dude, you probably got gluten somewhere and from a sauce or something like that that I came across and it caused me to have some type of symptom. So obviously that’s a huge cause that we always stay away from as much as possible, staying away from, you know, wheat protein, gluten. But there’s this–this whole list, I mean, that we could make a thousand–a thousand pages long of these other things. So if you’re getting frustrated and you’re thinking it’s that one piece of your life that’s causing you issues, maybe. But it could that we need to just focus in on several different pieces of your life at the same time and just take a few baby steps in the right direction to get your better.
Dr. Justin Marchegiani: Exactly. 100% agree. Now a lot of people are all about, “Well, how do I know I have leaky gut?” Well, there are some tests out there. I personally don’t do any of these tests because I think anyone that has digestive issues or has chronic health issues, they’re gonna have a leaky gut because there’s a common pattern in any of these patients. There’s inflammation. There’s maybe some food allergens. There’s poor digestion. There’s lack of stomach acid. A lot of times there’s an infection. There are maybe some toxicity overwhelm or overload. It may be some nutritional deficiencies. I mean, all of those together are gonna be like a perfect storm. So Cyrex through a lab, I think out in the west coast, that looks at some leaky gut markers like actomyosin, occludin, or zonulin and they look at lipopolysaccharide. That’s the endotoxins and look at the various antibodies and they’re kinda looking at the fact that these antibodies are gonna be a strong stimulating factor of leaky gut, especially if we know zonulin’s there, right? That’s the protein that kinda unzips that gut lining. So these are some more objective ways to quantify leaky gut. I don’t think you have to go that way. Most people don’t need that. They can just start with the general 5R plan and they’re gonna already start getting better and feeling better off the bat because with the whole leaky gut test, it doesn’t change anything in treatment. We’re not gonna go about doing anything differently because we see some of these markers pop up. So if it doesn’t change treatment for me, why do it? The only time–
Evan Brand: I love it.
Dr. Justin Marchegiani: Yeah, the only time I would do it is if someone’s kind of a biohacker and really wants objective data or someone’s just very skeptical and is like, “Well, I wanna see it. I wanna look at it. I wanna–I wanna touch and feel it and know that it’s actually there.”
Evan Brand: That–that’s so smart. I’m so glad you said that. Because like some of the other stuff, like a stool test, you can’t opt out of that. An adrenal test, you can’t opt out of that.
Dr. Justin Marchegiani: Uh-hmm.
Evan Brand: Organic acids, you can’t opt out of that.
Dr. Justin Marchegiani: Right.
Evan Brand: This one, you can pretty assume. I mean, what would say? Would say 9.9 out of 10 people that are having the symptoms we’re seeing are leaky gut people?
Dr. Justin Marchegiani: Absolutely and then it–it comes down to what degree as well, right? And that may be different from day-to-day and to, you know, what food exposure and what stress you’ve had and sleep and all that, so there’s a lot of variables. Another variable, another test that I think you can bypass on is food allergy testing. I don’t think food allergy testing is bad and for some people it may be a good idea especially if you’re dealing with someone that’s very resistant to cutting out foods and need to see it in black and white, like I mentioned with leaky gut. That can be helpful, but most people they’re gonna need an elimination diet with some level of rotation to it. Let’s think about it, right? If you get back a test that says you’re allergic to beef and chicken and a whole bunch of vegetables and fruit that you’re already eating and then you start eating, “Well, I’m gonna more fish and I’m gonna eat more–more turkey, and then I’m gonna eat these vegetables and these fruit.” And then you re-do the test, well, if the gut’s leaky, guess what happens? You tell me, Evan.
Evan Brand: I don’t–I–
Dr. Justin Marchegiani: In the spot.
Evan Brand: I honestly zoned out. I was so entranced with the tone of your voice that I got lost. Say it again?
Dr. Justin Marchegiani: Evan, that is 10 Paleo demerits. Alright, I want 25 push-ups right now. So basically, anytime you switch to the foods you’re eating especially early on with the gut still being inflamed, you’re gonna eventually develop antibodies and an immune response to the new foods you’re eating as well. So if you’re allergic to beef and you cut beef out and now you’re eating turkey every day, well, then it’s just a matter of time before turkey’s on that immune list.
Evan Brand: Right, was there a question involved in that?
Dr. Justin Marchegiani: So the whole idea is well, what do you do with the diet? Because if, you know, I’m not getting this food allergy test, well, how do I figure out what to eat? Well, typically a good elimination diet that involves an autoimmune Paleo aspect is usually a good starting place for most people and I always tell patients, “rotate their meat families,” so a good way to go is turkey–or I should say–your poultry, your fish, your beef, and your pork. Kinda rotate those proteins, pick one per day and rotate them and then eat different colors of vegetables. Different colors and you can even break it down to taxonomy of the vegetable family. I have a handout on my website that does that but for most people that aren’t terribly sick, just eating different colors and rotating the types typically is enough. The fats tend to be more benign because it’s the–the immune component in the body is more protein-based so having just fats tend to be okay. Again, butter has a little bit of casein, right? So butter may be an issue but pure coconut and pure olive oil tend to be fine. So moral of that story is an elimination diet with an autoimmune element that has some rotation pieces to it tends to be a better replacement for any food allergy testing.
Evan Brand: Yeah, just imagine if the whole world went on an autoimmune Paleo diet, how much money would be saved in the healthcare system overnight?
Dr. Justin Marchegiani: Oh, my God. I mean, just diabetes alone, it’s gonna bankrupt the healthcare system.
Evan Brand: Oh!
Dr. Justin Marchegiani: People don’t know it but the average life span of someone that’s diagnosed diabetic is like $2 million. You know, their–their life span of costs when frankly, I mean, this stuff can be fixed relatively easily with just some diet and some lifestyle and exercise pieces and maybe some–some supplementation as well. Like, I mean, a couple of thousand dollars gone.
Evan Brand: Yeah, I know. It–it’s just amazing to me. I mean, I’m kinda zooming out here in my head about all the different problems that we see and the different manifestations of where someone that’s just starting with this condition of leaky gut, how they start with this, but they could end up with an autoimmune disease and now they’re on Humera and these other immunomodulating drugs and they have the medical bills and then they have the side effects and they have the side effect of the side effect and it’s just amazing to think that there’s so many people going down the rabbit hole when just with this podcast here, I say this is probably one of the most important podcasts we’ve ever done because–
Dr. Justin Marchegiani: Uh-hmm.
Evan Brand: If you start here with this foundation of getting this gut lining and this tight junction in order–
Dr. Justin Marchegiani: Uh-hmm.
Evan Brand: You’re gonna save yourself potentially thousands of dollars and maybe even millions over your lifetime and the quality of life, I mean, that’s priceless. There’s no dollar–dollar sign that you can put next to that, so–
Dr. Justin Marchegiani: Absolutely, and just remember anyone who has an autoimmune condition, autoimmunity starts in the gut. Alessio Fasano, researcher out of University of Maryland now over at Harvard, he’s the one that kinda coined the term or did a lot of the research on gastrointestinal permeability and he was kind of, you know, almost a pariah in the field so to speak. I mean, Harvard’s now picked him up and he’s done a lot of great research but he got a lot of crap. I saw him speak at an autism conference a few years back and he was just lecturing to all the people saying, “Guys, you have no idea how much crap I’ve gone through just to bring this information to the forefront.” And I couldn’t believe it, because, you know, now leaky gut is even becoming more mainstream but this guy went through a lot of slings and arrows to bring this information up there and he’s even gone as far to say that this mechanism, leaky gut, gastrointestinal permeability has to be present in almost all autoimmune conditions for them to even happen to begin with. So that means your Parkinson’s and your MS may be driving–may be driven from a gut issue to begin with.
Evan Brand: Oh, man! That’s–that’s mind-blowing right there.
Dr. Justin Marchegiani: Wrap your head around that like something that’s not even GI-related is coming from the gut and this is where medicine, conventional medicine drops the ball because you are already alluded to it earlier, it’s like everything has like one, like a cure of symptoms–a cure of symptom and it’s just one thing. But you can’t cure something that has multiple causes. And there could be literally just 10 causes happening at once. Let’s say each cause has a 10%, you know, it’s 10% attributed to the underlying condition, well, it’s not just one thing to point at, you may have to treat each of those 10 things and knock each down from 10 to 0 for that person to get better. A drug can’t do that because it’s only focused on one enzyme system or one biochemical pathway that is blocking or inhibiting and it’s not fixing or upregulating any of the systems and it’s only focused on one at a time.
Evan Brand: Yup, yup. Well, that–that doctor that you were talking about, I mean, it’s a lot like what happened with Galileo. I mean, here he is discovering that the Earth is spinning around the sun, I mean, I don’t know this stuff full story but I’m pretty sure he was–I don’t know if he was imprisoned or at least highly, highly stigmatized for this discovery and everybody is like, “Yeah, right. You’re an idiot.” You know? The Earth does not spin around the sun. Something so revolutionary and he–it takes some, however, many years. I mean, he probably died before it actually comes out that that was true. I mean, when–you know, Newton and Coppernicus and all these other guys come around and they were like, “Yeah, he was right.” So it’s–it’s basically what’s happening now but it’s just in medicine. It’s this whole idea that we have to just–we have to invent the drug, right? It’s like we’re gonna find the cure. The cure is never going to come into–
Dr. Justin Marchegiani: Yeah.
Evan Brand: One pill. It’s not gonna happen.
Dr. Justin Marchegiani: Uh-hmm. No, it won’t. And then the same thing with Dr. Semmelweis who figured out that, you know, going from the autopsy lab where he was doing, you know, pathological dissections keeping the blood on his hands and not washing it and go and deliver babies upstairs was causing all kinds of, you know, illnesses with these newborns and causing death. And it’s like, my God, he came up with the idea, let’s change our gloves and wash our hands, and he was like exiled. It’s like, “You’ve gotta be kidding me.” Like if you were to–if you would go today and say, “Well, yeah, washing your hands is bad.” You’d be like, “What? Of course. You need to wash your hands especially in surgery.” And this guy was thought to be like a heretic, you know, just a little over a hundred years ago washing your hands was considered to be, you know, insane, which is just nuts in itself.
Evan Brand: So we’re living in the future right now. Like this podcast is ahead of its time. I mean, this stuff, not to toot our own horns too much here but I mean, it could take another–give–I mean, give me a timeline, I mean, you’ve been doing this stuff longer than me. How long is this gonna take to become mainstream where the doctor on every corner is talking about this stuff we’re talking about?
Dr. Justin Marchegiani: I don’t think it will happen from a top-down approach. It won’t happen with the drug companies or the conventional mainstream doctors because there’s–they’re too entrenched with the pharmaceutical model and too funded by it. With their education and their treatment modalities are 100% focused on symptom drugs. It’s allopathic. It’s great for acute medicine because the isolated cause of acute issues, they’re acute. They happen once. That’s the whole reason why they’re acute. The car accident patient who broke their leg. The car accident happened. It’s done. It’s over with.
Evan Brand: Yeah.
Dr. Justin Marchegiani: But the people that have the issues that we have, they’re having little micro car accidents every single day 24/7, and it’s not being fixed by the Celebrex that was prescribed or by the anti-depressants. So the medical model will never–it won’t–it won’t change top-down, meaning it’s not gonna be the government and the doctors and the drug companies that do it. It will just change based on a free market approach or people saying, “I’m gonna go look for a functional medicine doctor to fix my condition because my conventional doctor is just throwing anti-depressants and Prilosec and Nexium and corticosteroids at me and immune-suppressive drugs and it doesn’t look too good and the side effect’s staying and it’s not fixing any of the issues.” So we’re getting information out there and we’re just trying to create another option, so now instead of only having option A, which is drugs and surgery and–and trying to manage symptoms as they get worse where eventually the side effects become worse than the actual disease to begin with, we’re having a second option that’s more free market where you can actually get the underlying issue fixed and part of that issue is always gonna be the diet and the lifestyle and the nutritional piece which frankly isn’t even present at any medical schools.
Evan Brand: Not at all. Yeah. So the bottom-up approach, I mean this grassroots thing is happening now is just going to become an even bigger and bigger presence until it’s actually–whether it’s accepted or not, we don’t’ really care, I don’t care at least–so that bottom-up approach is just gonna get so big that it reveals itself because of the success rate that it has.
Dr. Justin Marchegiani: Yeah, it’s gonna be just natural inclination of people searching online, blogging, listening to podcasts, and getting tired of the options that are thrown at them from the medical establishment. I mean, the functional medicine community doesn’t have billions of dollars of marketing. What they really have are individual doctors and practitioners like myself that go out on the Internet and blog and do podcasts and do videos. That’s it. I don’t have a billion-dollar payroll to–to market this stuff. So for me, it’s just me putting free information out there, trying to give people hope and connect with them and give them solution. That’s it. That’s my marketing plan and lots of free information. That’s it. Now conventional medicine it’s a different–different story. You open up the–the TV, your–your paper, right? I mean or any magazine. Like drug commercials they’re just littered out through it and you’re not gonna see that in functional medicine.
Evan Brand: That’s very true.
Dr. Justin Marchegiani: Yup. So and they got functional medicine in the Cleveland Clinic now and now I’m already predicting that it will kinda be a watered down version of functional medicine. It will be functional medicine light or diet functional medicine, and I don’t think it will be, you know, what functional medicine could or–could be because well, I mean, frankly, if you got a massive multimillion-dollar hospital that makes a whole bunch of money, because they have cancer wards and heart disease wards and they treat diabetic patients, and you got this one department called functional medicine, that’s sucking all the other departments dry–dry, I mean, it–they’re a business that have to stay in. And if one part of it is losing money for the whole hospital, how could you stay in business? It’s not a viable model.
Evan Brand: Yup.
Dr. Justin Marchegiani: Right? If it’s by itself and it’s fully an entity onto its own like–like me and you are, it’s different. But when you are a hospital that makes hundreds and millions of dollars and you got one sector of that hospital causing every other sector to–to lose money, it becomes pretty tough.
Evan Brand: Yup.
Dr. Justin Marchegiani: So wrapping up here, Evan, is there anything else you wanna say before we give all the listeners kind of a–a Reader’s Digest summary here?
Evan Brand: I think this was good. I mean, this was definitely longer than some of the other episodes but this was well-needed and I think we covered a lot–a lot of ground here.
Dr. Justin Marchegiani: Yeah, so I think off the bat, we’re already ones coming in. The first thing you can do is try to eat your food in a non–at a non-stressful, stress-free environment, chew your food, one chew per tooth, right now I think that’s 32 chews if memory serves me right. Make sure you’re not drinking a whole bunch of water with your meals and avoid all the inflammatory things that are gonna be driving that zonulin stimulation. The gluten is gonna be the first. Any of the dairy outside of, you know, butter may be okay. All of the extra irritants and chemicals and pesticides, so go organic. And then if we’re having digestive issues, we wanna look deeper at infections. We wanna look deeper at SIBO and dysbiosis and H. pylori and low stomach acid and low enzymes and then if we are still having issues from there, the next step will be to really go through a 5R program with a–a good quality functional medicine doctor that really gets to the root of these issues and helps heal that gut and get your digestion optimal.
Evan Brand: Yup.
Dr. Justin Marchegiani: Anything else, Evan?
Evan Brand: That’s it. I mean, I’m sure I could rant some more but I think we’ve–I think we killed it today, my man.
Dr. Justin Marchegiani: Alright, man. You have a good weekend.
Evan Brand: You, too.
Dr. Justin Marchegiani: Bye.
Evan Brand: Bye.
[retweet]